We are thrilled to announce that we have raised $100 million in funding led by Enhanced Healthcare, to advance value-based care and strengthen primary care practices.
In spring 2022, we secured $50 million in series B funding to invest in care delivery infrastructure, evolve our business to support key evolutions in healthcare, expand our people resources and provide the best experiences for providers and patients.
We know primary care providers (PCPs) are their patients’ champions
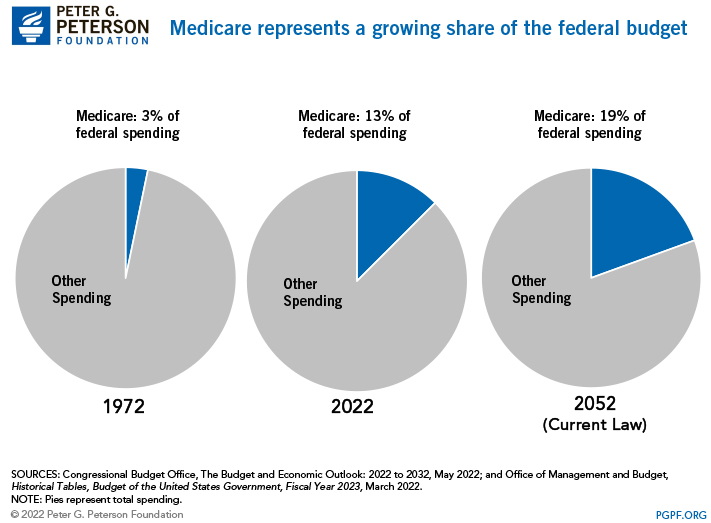
The current healthcare system has essentially taken the “health” out of healthcare, prioritizing volume over value. Though Medicare was created to improve both access to quality care and economic security, as the aging population continues to grow, healthcare spending in turn continues to increase. In fact, Medicare spending grew 8.4% to $900.8 billion in 2021 and this number is expected to exponentially increase as the entire baby boom generation reaches Medicare eligibility in 2030.
Instead of the traditional fee-for-service model where providers are paid for administering a multitude of services that have little to no impact on improving patient health outcomes, we incentivize wellness and whole-person health through value-based care. While independent PCPs often face financial challenges and additional difficulties like dealing with policy changes, and lack of access to data and analytics, we work to address those challenges and overcome barriers by providing smart data-driven solutions tailor-made for partner providers and patients.
Here is how we have accelerated value-based care and impacted patient experience in the last two years:
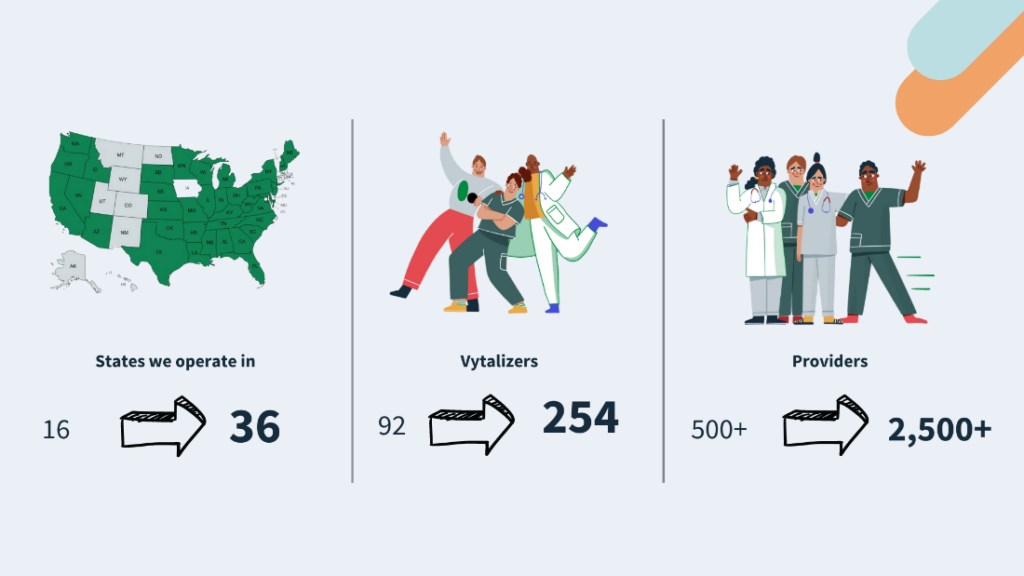
Growth and expansion to make a bigger impact
Saved $412 per patient in 2021 together with our partner providers
Expanded to 36 states
Partner with 2,500+ primary care providers
Entered into partnerships with hospitals, health systems and specialists for the first time
We empower practices with the tools needed to excel in value-based care
We know that most providers care deeply about quality but lack the necessary tools to surface potential care gaps that they may not see. At Vytalize, we empower providers to move past the apprehension that comes with leaving the comfort of fee-for-service behind, encouraging them to truly see the benefits of providing high-value care rather than lower value services.
Most ACOs approach value-based care as one size fits all, which can deter most providers from taking the leap because each practice has different needs. Addressing unique issues with a generic solution rarely improves patient outcomes. Providing an all-in-one solution tailored for each practice makes all the difference. Here are a couple of quick examples of activities that we do:
- We connect with our partner practices during weekly peer-to-peer meetings. During these meetings, we discuss pain points, share actionable data that allows them to be proactive rather than reactive and set them on a path to success.
- We use data and evidence-based medicine to enable our partners to keep their patients well and their practices thriving. For one partner in particular, data showed that palliative care was important for their practice. They used the data provided to implement changes, rolling out their own palliative care program.
- We monitor progress with key performance indicators (KPIs) known as Vytal Signs. Vytal Signs allow our partners to succeed in value-based care through high-value services like Annual Wellness Visits (AWVs) and Transitional Care Management (TCM). For AWVs, we have demonstrated that our partners reduce the total cost of care by $2,600 for patients who had an AWV. Further analysis shows that savings of $2,600 were created in years two and three as well for those patients who were up to date on their AWV. For TCM services, from 2021-2022, our programs saw a 13% reduction in hospital readmissions, saving more than $2.8 million.
Providing an all-hands-on-deck approach when and where providers and patients need it
Our Priority Care Program extends the practice’s reach to patients’ homes and incorporates social, economic, and other non-clinical factors in their environment, taking a holistic approach to care. This program leverages data to identify patients with the greatest needs.
Medicare’s Hospital Insurance Trust Fund, covering Part A, is projected to have a shortfall in 2029. At Vytalize, we’ve seen a 41% reduction in ER utilization and a 38% reduction in admissions for patients from our most engaged practices.
Recruiting the best of the best
162 of the best and brightest joined us to transform healthcare for the better.
Leadership Additions
We added innovative industry experts to our leadership team:
- Scott Weingarten, MD, Chief Value Officer
- Mark Long, Chief Technology Officer
- Derek Kang, Chief Compliance Officer
- Frank Bordonaro, Senior Vice President of Value-Based Care and Network Development
- Scott Segell, Executive Vice President, Value-Based Performance
- John Torontow, MD, Executive Vice President and National Medical Director
- Ken Stoll, Chief Payer Contracting
- Carina Unger, Vice President, People Operations
- Bernadette Minton, Vice President, Strategic Products
Drawing on the strengths of our unique work culture to guide Vytalizers supporting providers
Everything that stems from an organization is a product of its culture. Here is a taste of ours:
Our Mission: To accelerate the transition to value-based care for patients by taking care of the doctors who take care of us
Our Vision: To be the best facilitator of people’s healing through care that’s personalized, evidence-based and kind
Here are a few of our guiding values and principles that we share:
The last two years were full of growth for Vytalize. Join us as we continue to advance value-based care in the years to come.